March 22, 2022 submitted by South Shore Health (courtesy photos)
March is National Colorectal Cancer Prevention Month, a good time to spread awareness about the disease and the importance of colorectal cancer screening, prevention and treatment. This series asks experts in five cancer specialties – breast, colorectal, gynecologic, lung, and prostate – five questions focused on wellness, prevention, and the crucial screenings that help save lives.
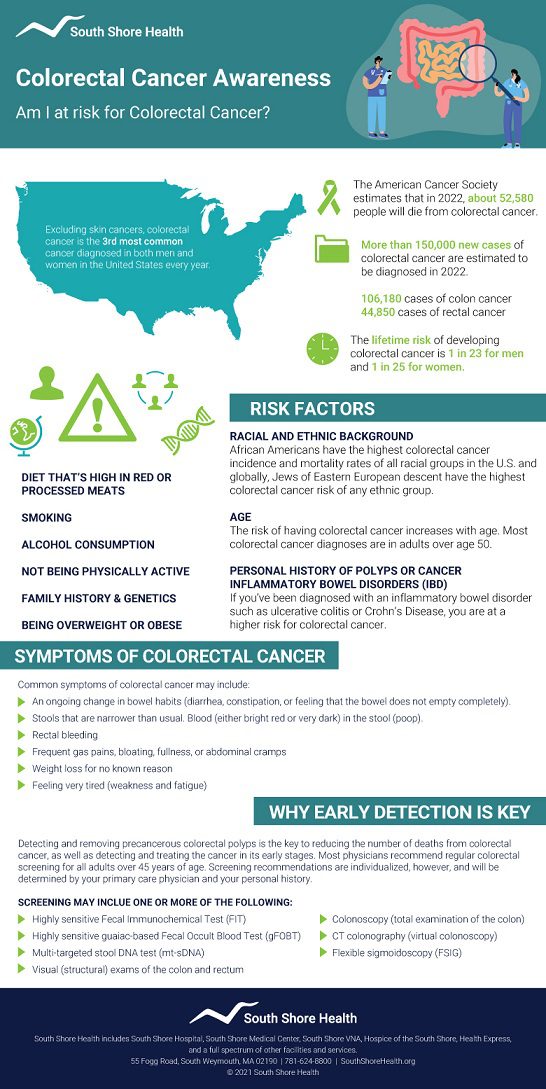
Colorectal cancer is the third most common cancer (other than skin cancers) diagnosed in both men and women and the third leading cause of cancer-related deaths in the U.S.
According to the American Cancer Society (ACS), 106,180 new cases of colon cancer and 44,850 new cases of rectal cancer will be diagnosed in 2022, and 52,580 people will die from the disease.
While the lifetime risk of developing colorectal cancer is 1 in 23 for men and 1 in 25 for women, both the overall rate of diagnoses and deaths have dropped over the last several decades. The ACS attributes the decrease due to more screening, improved treatment and awareness about lifestyle-related colorectal cancer risk factors.
Screening through colonoscopy can help find colorectal polyps so they can be removed before they can develop into cancer and also detects cancers at an earlier stage when they are easier to treat.
Robert Driscoll, MD, a surgeon at Brigham and Women's Harbor Medical Associates in Braintree answers five common questions on colorectal cancer screening, prevention and treatment.
When it comes to colorectal cancer prevention, how important are routine or annual screenings?
Routine screening for colorectal cancer and modification of risk factors has substantially decreased both incidence and mortality from colorectal cancer.
What kind of screening is available for colorectal cancer and at what age should people start being screened?
For patients at average risk for colorectal cancer, regular screening should begin at age 45. There are two types of screening available – stool-based testing and structural or visual-based testing through colonoscopy.
Stool-based testing is done yearly unless there is a positive test. Those patients should then undergo visual testing. Visual testing is performed at 3-to 5-year intervals, depending on the findings.
People at increased risk for colorectal cancer should be screened earlier than age 45. Screening for this is individualized both for frequency and type of testing.
What are some of the risk factors for colorectal cancer and are there lifestyle or diet changes that can lower someone’s risk?
There are several risk factors associated with the development of colorectal cancer. The risk factors that are modifiable include obesity, physical inactivity, a diet high in red meat, smoking and alcohol use.
Unmodifiable risk factors include age, a history of inflammatory bowel disease, inherited syndromes -- such as Lynch Syndrome, a family history of colorectal cancer or adenomatous polyps, familial adenomatous polyposis, and Type 2 diabetes.
Certain ethnic groups also have a higher incidence of colorectal cancer – particularly African Americans and Eastern Jewish groups.
What are some of the symptoms of colorectal cancer that someone should be concerned about and discuss with their primary care provider or specialist?
Concerning symptoms of colorectal cancer include changes in bowel habits, feeling the need to have a bowel movement but not feeling relieved by having one, rectal bleeding, weakness, fatigue, unexpected weight loss, cramping or abdominal pain.
What kind of treatment options are available for someone diagnosed with colorectal cancer?
Treatment options for source control center largely on surgical resection. Some early cancers can be treated with a minimally invasive or endoscopic treatment, with resection of the malignant polyps or removal of the tumor.
Usually, however, surgical resection of the involved section of the bowel will be needed. For more advanced cancers and cancers in certain parts of the intestinal tract (rectum), combined treatment with radiation, chemotherapy and resection is needed.
Robert P. Driscoll, MD, is a surgeon at Brigham and Women's Harbor Medical Associates in Braintree. Learn more about colorectal cancer care at Dana-Farber Brigham Cancer Center in clinical affiliation with South Shore Hospital.